What Medicare Issue Was Fixed In 2020: In terms of health care, what impact would the 2020 contenders’ policies have on coverage? Since the Affordable Care Act was signed into law in 2010, the percentage of Americans without health insurance has decreased by more than half. Despite this, 30 million people remain uninsured, and even those with health insurance may still struggle to pay for care.
A number of politicians and elected figures, most notably Donald Trump, propose policies that would lower the generosity of government insurance programmes and federal spending while simultaneously reducing the number of individuals who have health coverage. By extending federal health care programmes and boosting federal spending, some politicians, mainly Democrats, support policies that would help the uninsured. The scope of these plans varies greatly.
Both Republican Senator Tim Scott of South Carolina and Democrat Congressman Ron Kind of Missouri introduced the legislation this year, in both houses of Congress. Senate Majority Leader Tim Scott said, “Today, the PAID Act has moved a key step closer to becoming law, patching up Medicare-related potholes that have cost seniors, Main Street job creators, and the American taxpayer millions of dollars over time.” We can benefit seniors and families around the country by reducing obstacles caused by out-of-date regulations and bureaucratic red tape that have plagued the MSP for far too long.
This section contains the most important information you need to know
From President Trump’s plan to replace the Affordable Care Act (ACA) with a single-payer system to proposals from some Democratic presidential candidates, there is a wide range of ideas on how to reform the American health care system. In some cases, these plans differ from one another because policymakers have distinct goals, and in other cases, they disagree on the best way to accomplish the same goals. This article provides an overview of the current state of health care in the United States, as well as how some of the most notable ideas might alter that situation.
Currently, how Americans obtain medical insurance
More than 90% of the population in the United States is now covered by some form of health insurance plan or another. More than half of Americans have health insurance through their employer or a family member, but it’s not universal. Medicare, which covers seniors and some individuals with disabilities, and Medicaid, a combined state-federal programme that covers low-income people, account for another 17 percent of the population.
5 percent of Americans buy insurance on the individual market, either by using the ACA’s Marketplaces or directly from an insurance carrier. Nine percent of the population nearly 30 million people don’t have health insurance. Most people who buy individual market insurance are able to do so because of the ACA, which has reduced the number of people without health insurance by more than two-thirds since its implementation. Individuals’ insurance status can change over time; those who have insurance now may lose it or get new coverage, while those who are now uninsured may do so in the future. This means that anyone who wants to know how a policy will affect them must take into account not just the coverage they currently have, but also the coverage they may get in the future.
Do proposed reductions in the generousness of federal healthcare programmes have an impact on the availability of health care?
Many Republicans in Congress, including President Trump, have proposed reducing government money for programmes that subsidize health insurance for low- and middle-income Americans and eliminating regulations that apply to private insurers, two frequently debated ideas. Some of these suggestions would reduce federal spending on health care while increasing the number of uninsured people and increasing costs for sick individuals, while lowering the cost of health insurance for some healthy individuals, in general.
As a result of the PAID Act’s amendment, the growing number of lawsuits brought by Medicare Advantage Plans alleging recovery rights against insurers, including claims for “double damages” under Medicare’s private cause of action provision, will be effectively settled. A better resolution and repayment of MSP liabilities related to settlements, judgments, or awards can be achieved if CMS provides settling parties with the name and identity of the plan and the months of coverage.
How single-payer system affect health coverage in USA?
Most Democratic candidates and elected officials, in contrast to policymakers who are focused on cutting spending, support policies that will expand government programmes (and spending) in order to cover all of the uninsured people. “Single-payer” healthcare is supported by some Democratic candidates and political leaders, as opposed to the patchwork of coverage sources we currently have.

What other options do we have outside a single-payer system that could help us get more people covered for health care?
Single-payer schemes have not been adopted by all Democrats and even many proponents of such a plan favor more limited plans. The focus of these plans is on those who are already uninsured or who suffer exceptionally high expenses, rather than aiming to change the method that all Americans obtain insurance. In most cases, they are aimed toward preserving current employer-sponsored coverage. There is a wider range of options here than in the single-payer debate. As illustrated in the chart below, the Urban Institute expects that the number of uninsured individuals will rise among particular groups of people.
Fixing Medicare Secondary Payer Gap with PAID Act Becomes Law In the 17th year of 21st century
To keep the government running, the PAID Act was signed into law on December 11th as part of the finance measure. The PAID Act, which was introduced in 2019 and has been a primary focus of RIMS Advocacy, will correct a present gap in MSP compliance. As per 42 U.S.C. 1395y(b)(8)(G) of the PAID Act, the Centers for Medicare and Medicaid Services (CMS) must expand their Section 111 Query Process in order to determine whether a claimant is currently eligible for Medicare Part C (Medicare Advantage) and/or Medicare Part D (prescription drug) benefits or has been eligible for those benefits in the preceding three years.
Thirty-One Facts About Medicaid Supplemental Insurance in 2020
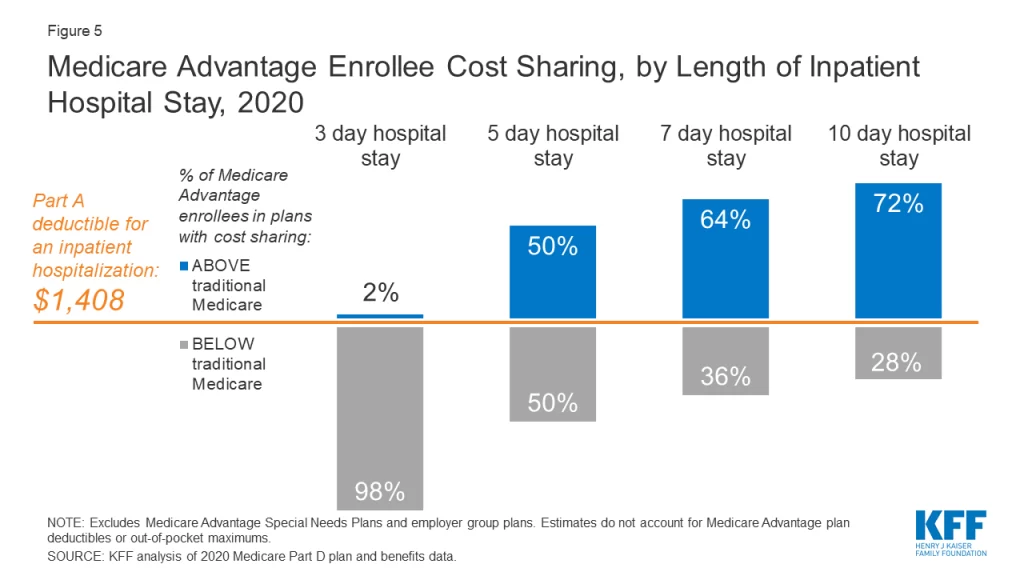
Advantage plan participation has skyrocketed in the last decade, and these programmes are now playing a larger role in the overall Medicare programme. Medicare Advantage enrollment, rates, and out-of-pocket maximum information are all included in this data study. In addition, an analysis of the additional benefits and authorization requirements of Medicare Advantage plans is included. Additionally, the analysis focuses on Medicare Advantage coverage modifications made in 2020 as a result of the COVID-19 epidemic.
By 2020, approximately 40% of all Medicare beneficiaries – 24.1 million out of 62.0 million – will be enrolled in Medicare Advantage plans, a percentage that has gradually risen since the early 2000s. This represents a significant number of people. About 2.1 million beneficiaries, or 9%, were added to Medicare Advantage between 2019 and 2020, the same growth rate as the previous year. More than half of all Medicare enrollees will be enrolled in Medicare Advantage plans by 2030, according to the Congressional Budget Office (CBO).
Lower reimbursements for healthcare providers and pharmaceutical companies, as proposed by a single-payer system, will alter the market for healthcare services, including how providers offer treatment and how pharmaceutical companies design new drugs. If the public option is offered at a lower price and a larger percentage of the eligible population chooses it, this could have different implications.