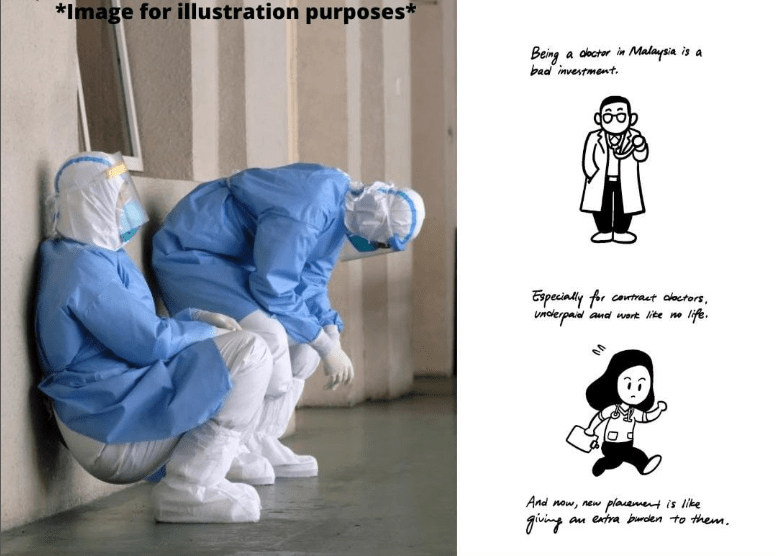
Medical Officer Leaving Hospital Is Amusing: As Covid-19 increases, hospitals in half of the states are suffering a severe staffing shortage, Prompting the statement, “People are going to die.” Health care facilities in at least 25 states face serious staff shortages as the number of coronavirus cases continues to rise, according to a trade association and STAT.

A shortage of beds has led to the transfer of patients from Texas to Arizona and central Missouri to Iowa, where they’ve had to travel hundreds of miles to find a bed. Many of these hospitals spent months stockpiling medical equipment and protective clothing in reaction to Covid-19, but without appropriate staffing, the items are of little value. “Care is more than just a hospital bed in a room. Texas Organization of Rural & Community Hospitals CEO John Henderson says it’s about doctors taking care of patients (TORCH). In the absence of adequate staff, “people will die.”
Multiple regions face major staffing shortages. There is a shortage of intensive care unit nurses in some regions of Texas, so they’re taking on six to eight patients at once, says Robert Hancock, president of the Texas College of Emergency Physicians. According to spokesperson John Palmer, 20% of the 240 institutions affiliated with the Ohio Hospital Association are reporting staffing shortages.
President of the American Hospital Association, Nancy Foster, said she has heard from more than a dozen hospital chief executives in recent weeks, warning her of staffing shortages in places like Texas, North and South Dakotas, Minnesota, and Wisconsin. According to local reports from New Mexico to Wyoming to Tennessee to Georgia and Alabama to Indiana and Montana to California, Rhode Island, and South Carolina, health care practitioners across the country are reporting the same issue.
The Shortages are Exacerbated
As the coronavirus continues to spread, the shortages are exacerbated by an influx of patients, as well as a decrease in the number of staff members who are ill or are quarantined after being exposed to infected people. For years, rural areas have been plagued by a dearth of health care workers, which has resulted in many rural hospitals being unable to care for critically ill patients due to a lack of equipment, such as ventilators.
As multiple states are struck simultaneously, systems designed to alleviate shortages by bringing in backup from other locations are unable to work. A nationwide shortage of doctors and nurses has left states that dispatched medical personnel to New York City early in the pandemic with nowhere to turn. Early on, Texas sent caregivers to New York to cope with the influx of patients, Henderson said. There are 48 states in crisis, and you can’t do that when they’re headed on the wrong path. “Where do you get your energy from?
A growing number of healthcare organizations are struggling to transfer patients in need of immediate attention to hospitals that can provide acceptable care. Several patients in Lubbock, Texas, were flown to Arizona because of the severity of their Covid-19, according to Henderson. According to Alex Garza, who heads the St. Louis regional pandemic task force and is the community health officer at SSM Health in St. Louis, a Missouri patient who urgently needed surgery to remove a mass from his brain was sent to an Iowa hospital for treatment. According to Henderson, “The mechanics of how you convey and expedite care are currently faulty.”
Upon admission, what happens next?
Patients were arriving in “very bad condition” in the early days of the pandemic, according to the anesthesiologist and assistant professor Benjamin Salter at Mount Sinai Health System in Manhattan, when the majority of hospitals, particularly those in the New York City area “were made up of a lot of ICUs. Rural hospitals in Texas are obliged to treat patients who would otherwise be sent to larger centers due to a lack of staff in even the state’s largest cities, such as Houston, Dallas, and Austin.
What if your condition worsens: “Watching your symptoms to see if they truly grow worse” and keeping an eye on “new symptoms that are super-concerning” are two of the most important aspects of care for patients in a COVID unit, says McKoy.
Are you going to put me on a ventilator: Respiratory difficulties do not necessitate intubation and placement on a ventilator—a machine that transports air into and out of the patient’s lungs by way of a tube.
Another thing to keep in Mind: Consider how you might help researchers better understand the coronavirus if you’re in the hospital. In the spirit of furthering research, McKoy recommends talking to your doctor about the potential of participating in a clinical study. Even if you are young and healthy, be sure you have your advanced instructions in place. (Zolpidem) McKoy argues that rather than seeing this as a burdensome duty, it should be viewed as a source of empowerment. In the event that you are unable to communicate your desires to doctors, advance directives are documents that outline the types of medical care you would and would not prefer.
As a doctor, you’ll need these 5 Qualities in order to Succeed
When it comes to your knowledge, you’re not scared to accept that you don’t know everything there is to know. The ability to declare “I don’t know” when there are gaps in one’s understanding or a lack of information is an important quality of a good doctor. You’re more than simply a textbook whiz. Emotional intelligence is a strong suit of yours. Doctors often make the wrong diagnosis because they’ve become accustomed to following a script of questions and answers and have missed red flags and signals that the problem may be more complex.
Your listening and observation skills are exceptional: According to Procure Proton Therapy Center Medical Director Gary Larson, “If you listen to the patient, they will tell you what’s wrong with them. “The majority of patients have also done some research online.” Dr. Smith referred you to me because he wanted you to learn more about your illness and the treatment options available to you.’
You’re a stickler for Perfection
There is no guarantee that every patient will appear with a condition that is immediately recognizable. Rare situations necessitate lengthy consultations with specialists, as well as several chats with the patient, multiple treatment plans, and multiple testing in order to arrive at a correct diagnosis. You have faith in your own judgment. While it’s always a good idea to do multiple tests to rule out dangerous illnesses, you shouldn’t run every medical test under the sun just for the sake of safety. For junior doctors, one of the most difficult obstacles is the inability to put their faith in their own judgment. Suzanne Koven, a doctor at Massachusetts General Hospital, says in a letter to her younger self and to all other junior doctors: “My dear young colleague, you are not a phony.
What’s next?
NHS has prepared a brief quiz to see if you have what it takes for a career working in the health care field. Why not apply to the MBBS program at the University of Central Lancashire if you’ve already made up your mind? An undergraduate degree in five years can put you in good stead for a variety of jobs in the continually evolving field of health care. Patient contact begins in your first year of study, and clinical assignments continue throughout your degree and into your final year. The curriculum was developed in response to input from clinicians and patients. A clinical skills suite and a human anatomy learning center are just two of the excellent facilities available for students to learn in small, diverse classes…