What is Pancreatitis: Because it is so difficult to detect, pancreatic cancer frequently only becomes apparent after it is already quite advanced. Two of the most prevalent signs and Symptoms of pancreatic cancer are jaundice and weight loss. Both diabetes and exposure to particular chemicals are risk factors. The type of treatment depends on the tumor’s size, location, and if it has spread to other areas of the body.
https://en.wikipedia.org/wiki/Pancreatitis
What are the benefits of the pancreas?
A hockey stick-shaped organ, the pancreas is situated behind the esophagus. The pancreas is primarily in charge of promoting healthy blood sugar levels and assisting with digestion. The pancreas releases glucagon and insulin to control excessively high or low blood sugar levels.
What is pancreatic cancer?
The pancreas cells undergo changes (mutations), which lead them to proliferate out of control and develop cancer. The likelihood of tissue buildup exists. This bump occasionally might be cancerous (not cancerous). However, with pancreatic cancer, the mass is malignant (cancerous).
Which types of pancreatic cancer exist?
The two types of pancreatic tumors that are most frequently found are exocrine and neuroendocrine tumors. Adenocarcinoma is the most common form of pancreatic cancer, and exocrine tumors make up 93% of pancreatic tumors. Most frequently, pancreatic adenocarcinoma is meant when someone claims to have pancreatic cancer. Ductal adenocarcinoma, which develops in the ducts of the pancreas, is the most common type. The other 7% of pancreatic tumors are neuroendocrine tumors (NETs), sometimes referred to as pancreatic NETs (PNETs), islet cell tumors, or islet cell carcinoma. Some NETs overproduce certain hormones.
Who develops Pancreatic Cancer?
According to the American Cancer Society, pancreatic cancer accounts for about 3% of all malignancies and 7% of all cancer-related fatalities in the country. Men are slightly more likely than women to experience it. Physical and psychological symptoms are the two different categories. Symptoms AND CAUSES OF THEY
Is there a cure for pancreatic cancer?
For extended periods of time, pancreatic cancer frequently stays unnoticed. As the illness worsens, it’s probable that people will recognize it.
- Upper abdominal pain that may radiate to the back.
- the fading of the skin’s color and the eyes’ whites (jaundice).
- Tiredness.
- being unable to eat.
- Poop has a pale color.
- Dark-colored urination.
- dropping in weight
- clots that form in the blood.
- Red, inflamed, and itchy skin.
- a brand-new or worsening diabetes variant
- Nausea and diarrhea
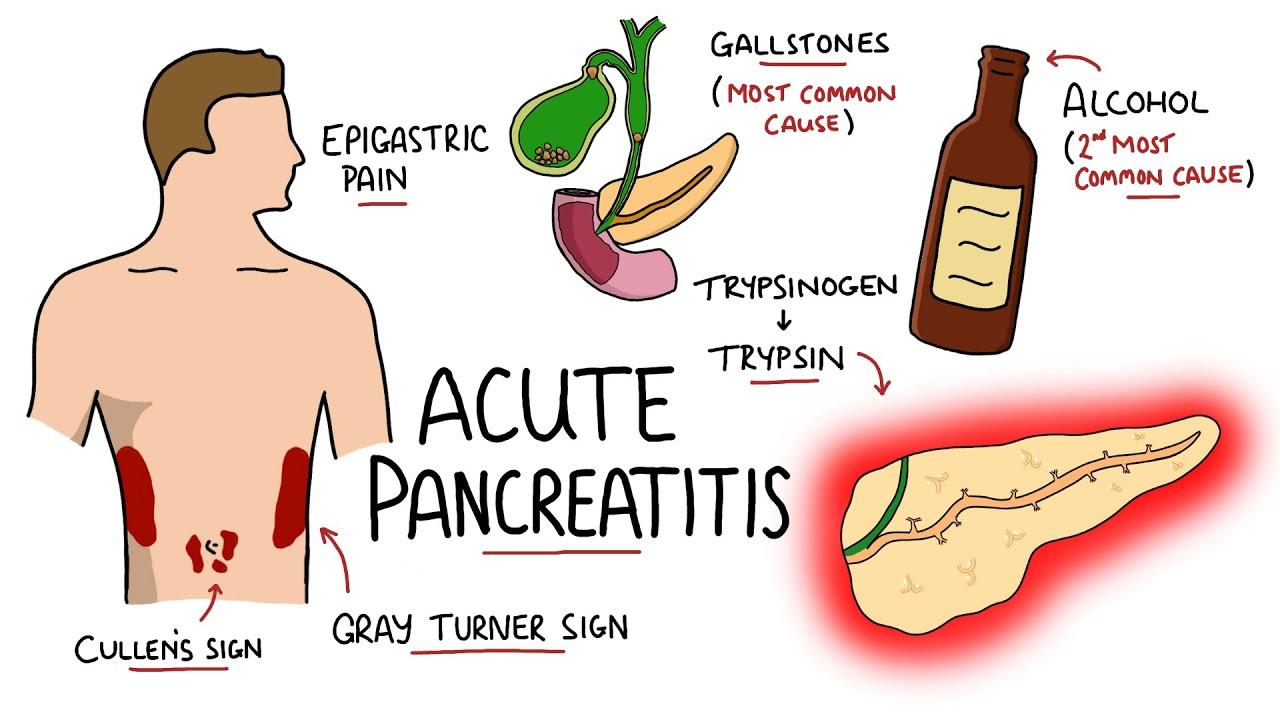
Based on your symptoms and the pancreatic inflammation, your doctor may suspect pancreatic cancer if you recently developed diabetes or pancreatitis. The signs and symptoms of pancreatic neuroendocrine cancer may not be the same as those of traditional pancreatic cancer, such as jaundice or weight loss. Hormone-producing PNETs are to fault for this.
Causes of pancreatic cancer include:
There isn’t a fix that works for everyone. Uncertainty surrounds pancreatic cancer. There have been certain risk factors identified, nevertheless. Flaxseeds, salmon, and tuna are excellent suppliers of these nutrients. According to a few small studies, omega-3 fatty acids have been associated with tissue repair and a reduction in inflammation in cases of pancreatitis. Eight clinical trials involving a total of 364 patients with severe acute pancreatitis were conducted. Some of the patients received omega-3 fatty acid supplements. Most folks weren’t, though.
Factors raise the risk of developing Pancreatic Cancer
Pancreatic cancer will eventually be discovered in one in every 64 individuals. You must have one or more risk factors in your life in order to have a higher risk of developing a disease. Risk factors related to behavior can be changed.
Food intake and Diet:
Doctors may advise patients to fast for several hours or even days during a flare-up. The goal of this drug is to lessen pancreatic inflammation. Malnutrition can result after severe pancreatitis, especially in the patient. Parenteral feeding is essential for the survival of many people. Medical practitioners inject an IV drip into a vein and provide nutrition through it.
Some of the risk elements for pancreatic cancer include the following:
- Most people smoke cigarettes, cigars, and other tobacco products.
- Another risk factor is obesity. The size of a person’s waist is a risk factor even if they are not obese.
- Type 2 diabetes, which is more frequent than type 1, is at risk due to obesity. Diabetes is a person with a normal BMI and at an advanced age could be a sign of pancreatic cancer.
- exposure to the chemicals that metal workers and dry cleaners use.
- An ongoing pancreatic inflammatory disorder is known as pancreatitis chronicles.
Some things, including risk factors, are beyond your control. These are but a few illustrations:
- Chronic pancreatitis is caused by genetic defects and passed down from parent to child.
- alterations in genes, such as the BRCA gene mutations, that are handed down from one generation to the next.
- having turned 45 years old.
- the simple fact that I’m a man
- the skin of a dark color.
- Jewish ancestry of Ashkenazi descent.
- Your doctor might suspect pancreatic cancer if you’ve lately developed diabetes or pancreatitis.
As soon as your doctor gives the all-clear, start eating smaller, more frequent meals. A low-fat diet that forbids greasy, fried, and processed foods aid in easing discomfort and preventing new episodes. because eating a lot of fat causes your pancreas to produce more digesting enzymes. An attack could be started by excessive enzyme levels.
A DIAGNOSTIC PROCESS AND TESTING PROCESS
Pancreatic cancer diagnoses: Early-stage pancreatic cancer is challenging to find. This is because a typical exam prevents doctors from feeling pancreatic. If your doctor believes you have pancreatic cancer, an imaging test may be prescribed. An endoscopic ultrasonography procedure is still an option. Endoscopic ultrasonography (EUS), as the name implies, uses a camera attached to a tiny tube that is introduced into the stomach through the patient’s mouth.
The pancreas can be imaged via the stomach wall using an ultrasonic probe linked to the distal end of the endoscope. If required, a pancreatic biopsy (tissue sample) under ultrasound guidance might be performed throughout the surgery. Blood tests can be used to find tumor markers. When it comes to pancreatic cancer, a high level of carbohydrate antigen (CA) 19-9 may be a sign of a tumor. To find out if there is a hereditary component to the disease, newly diagnosed pancreatic cancer patients should discuss with their doctor the option of genetic counseling and testing.
Location of pancreatitis discomfort
Pancreatitis patients may have excruciating upper abdominal discomfort that travels to the back. The discomfort could be brief, ongoing, or very bad. While acute pain might occasionally continue for a few minutes or hours, chronic pain can last for years. Upper abdominal pain after eating or while trying to fall asleep is more common in patients with pancreatitis. Early therapy makes it much simpler to recover fast and to experience symptoms again.
Summary:
Pancreatitis, a disorder that occurs when the pancreas gets inflamed, is quite painful. In extreme cases, it can be fatal. One’s way of life may need to be modified in certain ways to lessen discomfort and the possibility of recurrence. Limiting alcohol use, consuming less coffee, and following a low-fat diet are some examples of these lifestyle changes. The use of vitamins in the treatment of pancreatitis may help patients experience pain relief, stay healthy, and live longer. It’s too soon to say whether these treatments will benefit someone with pancreatitis.




